Snoring and sleep apnea are common sleep disorders that can significantly impact an individual’s quality of life and overall health. As an ENT surgeon, I understand the importance of exploring effective treatment options to alleviate these issues and improve patients’ well-being.
Introduction to Snoring and Sleep Apnea
Snoring is the harsh sound that occurs when airflow is partially obstructed during sleep, resulting in vibration of the tissues in the throat. On the other hand, sleep apnea is a more serious condition characterized by pauses in breathing or shallow breathing during sleep. These interruptions in breathing can occur multiple times throughout the night, leading to fragmented sleep and decreased oxygen levels in the body.
Understanding the Causes
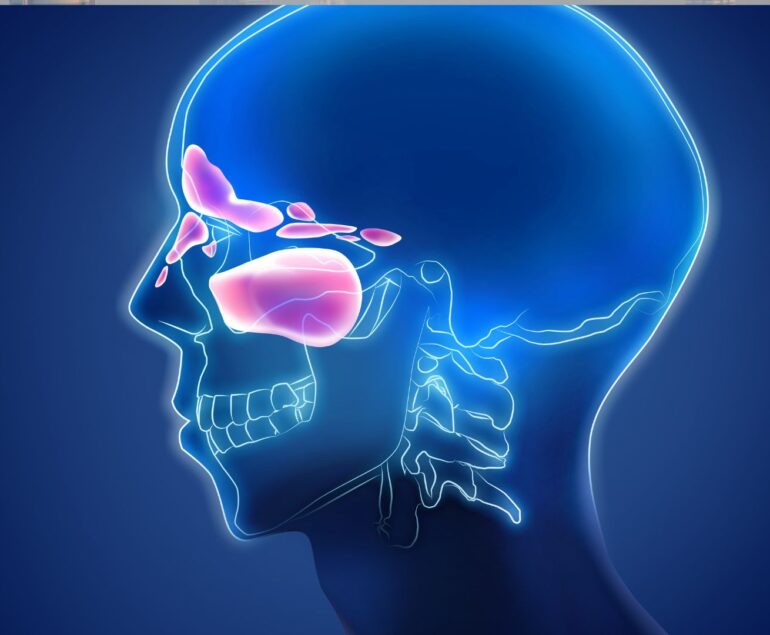
Anatomy of the Upper Airway
The anatomy of the upper airway plays a crucial role in the development of snoring and sleep apnea. Factors such as enlarged tonsils, a deviated septum, or excess tissue in the throat can contribute to airway obstruction during sleep.
Common Risk Factors
Several risk factors can increase the likelihood of developing snoring and sleep apnea, including obesity, age, smoking, and alcohol consumption. Additionally, certain medical conditions such as nasal congestion, allergies, and anatomical abnormalities can exacerbate these sleep disorders.
Impact on Health and Quality of Life
Health Risks Associated with Sleep Apnea
Untreated sleep apnea can have serious consequences for health, including an increased risk of hypertension, heart disease, stroke, and diabetes. Moreover, it can negatively impact cognitive function, leading to daytime drowsiness, difficulty concentrating, and memory problems.
Effects on Daily Functioning
The disruptive nature of snoring and sleep apnea can also affect daily functioning and interpersonal relationships. Chronic fatigue and irritability can impair job performance and strain personal connections, leading to decreased productivity and overall dissatisfaction with life.
Diagnosis of Snoring and Sleep Apnea
Accurate diagnosis is essential for determining the most appropriate treatment approach for snoring and sleep apnea. This typically involves undergoing a sleep study or other diagnostic tests to evaluate breathing patterns and oxygen levels during sleep.
Non-Surgical Treatment Options
While surgical intervention may be necessary in some cases, non-surgical treatment options are often explored as initial management strategies. Lifestyle modifications such as weight loss, smoking cessation, and positional therapy can help reduce symptoms and improve sleep quality. Additionally, continuous positive airway pressure (CPAP) therapy involves wearing a mask connected to a machine that delivers a steady stream of air to keep the airway open during sleep.
Surgical Treatment Options
When conservative measures fail to provide adequate relief, surgical intervention may be recommended to address anatomical abnormalities or structural issues contributing to snoring and sleep apnea. Various surgical approaches can be employed, depending on the specific needs and preferences of the patient.
Overview of Surgical Approaches
Surgical treatment options for snoring and sleep apnea aim to widen the airway and reduce tissue obstruction to improve airflow during sleep. These procedures may involve removing excess tissue, repositioning anatomical structures, or implanting devices to support the airway.
Types of Surgeries for Snoring and Sleep Apnea
Common surgical procedures for snoring and sleep apnea include:
- Uvulopalatopharyngoplasty (UPPP)
- Septoplasty
- Turbinate reduction
- Palatal implants
- Genioglossus advancement
Each of these surgeries targets specific areas of the upper airway to address underlying issues contributing to snoring and sleep apnea.
Benefits and Risks of Surgical Treatment
Surgical treatment for snoring and sleep apnea can offer significant benefits, including improved sleep quality, reduced daytime symptoms, and decreased health risks associated with untreated sleep apnea. However, it’s essential to weigh these potential benefits against the risks and potential complications of surgery, which can vary depending on the type of procedure performed.
Recovery Process and Post-Operative Care
Following surgical treatment for snoring and sleep apnea, patients will require a period of recovery and post-operative care. This may involve managing pain and discomfort, adhering to dietary restrictions, and avoiding strenuous activities that could disrupt the healing process. Additionally, patients should follow up with their healthcare provider to monitor progress and address any concerns during the recovery period.
Lifestyle Changes to Support Treatment Results
In addition to surgical intervention, adopting healthy lifestyle habits can further support treatment outcomes and long-term success in managing snoring and sleep apnea. This may include maintaining a healthy weight, avoiding alcohol and sedatives before bedtime, and practicing good sleep hygiene to promote restful sleep.
Importance of Follow-Up Care
Regular follow-up appointments with a healthcare provider are essential for monitoring progress, adjusting treatment as needed, and addressing any lingering symptoms or complications. Open communication between patients and healthcare providers is key to ensuring optimal outcomes and ongoing support throughout the treatment process.
Patient Success Stories and Testimonials
Sharing patient success stories and testimonials can provide valuable insight and encouragement for individuals considering surgical treatment for snoring and sleep apnea. Hearing firsthand accounts of improved sleep quality and restored health can inspire hope and confidence in pursuing treatment options.
Conclusion
In conclusion, surgical treatment options offer effective solutions for addressing snoring and sleep apnea, improving sleep quality, and enhancing overall health and well-being. By understanding the causes and consequences of these sleep disorders and exploring the various treatment modalities available, individuals can take proactive steps to regain control of their sleep and enjoy a better quality of life.
FAQs
- How do I know if I need surgery for snoring and sleep apnea?
- Your healthcare provider will evaluate your symptoms, medical history, and diagnostic test results to determine if surgical intervention is necessary.
- What are the potential risks of surgical treatment for snoring and sleep apnea?
- Risks and complications of surgery may include bleeding, infection, pain, and changes in voice or swallowing.
- Is surgery the only option for treating snoring and sleep apnea?
- No, there are various non-surgical treatment options available, which may be sufficient for managing mild to moderate cases.
- How long does it take to recover from surgery for snoring and sleep apnea?
- Recovery times can vary depending on the type of procedure performed, but most patients can expect to resume normal activities within a few weeks.
- Will surgical treatment eliminate snoring and sleep apnea completely?
- While surgery can significantly reduce symptoms and improve sleep quality, it may not completely eliminate snoring or sleep apnea in all cases.
About Author:
Dr. Vivek Kumar Pathak: Renowned ENT Surgeon, Senior Professor, and Founder.
Dr. Pathak, ENT surgeon at Kailash Hospital, Senior ENT Professor at Sharda University, and founder of Entegrity Care, brings expertise and innovation to healthcare. Discover the visionary behind Doxtreat Healthcare, shaping the future of ENT care.
Website www.drvivekpathak.com
Call +917838450942
WhatsApp +91 78384 50942
Book an appointment with Dr. Vivek kumar Pathak by filling the form.